On this page
What is population health management?
Population health management (PHM) helps us to improve the health and wellbeing of people living in Hertfordshire and West Essex (HWE) by using information about individual people and communities to understand local health and care needs, and how these vary for different populations. We can also use it to make sure the right services are in place to meet people’s needs now and what these might be in the future.
Population health management help our ICS to improve Population Health which is about the physical and mental health of our communities. This includes promoting wellbeing and reducing health inequalities, often linked to wider determinants of health, such as housing and education.
By understanding the needs of our population, health and care organisations working across our ICS can design, deliver and manage health and care services so they’re more joined-up and sustainable.
We can also use PHM to identify individual people with health and care needs who might benefit from specific interventions. The support received might be medical but can also be social, such as support with housing and employment, which can impact physical and mental health.
Visit the NHS website for more details on population health management.
You can access local insight packs for our population via the navigation options that at the bottom of this page.
We will continue to update this page with more detailed reports on the health outcomes based on the types of illness affecting those living in HWE.
You can view general health reports for Hertfordshire and west Essex by district on the Hertfordshire Health Evidence website.
PHM Offer for Hertfordshire and West Essex
Our PHM Offer operates in conjunction with the HWE Population Health Management Strategy. Our offer details the support that is available to different parts of the system, ensuring that teams are supported to deliver their objectives and achieve improved outcomes for the HWE population through the PHM approach.
PHM Strategy
1. Introduction and strategic context
The purpose of this strategy to describe the tools, resources and activities needed to embed a PHM approach within the local health system, enabling more informed decisions and delivering care that most effectively and efficiently meets the needs of the population.
PHM is the systematic use of data and intelligence in health system planning to deliver maximum impact on health outcomes, inequalities and value. The HWE Integrated Care Board (ICB) PHM Strategy describes the current level of PHM maturity within HWE, outlines a proposed future state that embeds PHM tools, techniques and approaches into its work and describes the steps to be taken to move from the current to the future state which may be influenced by national strategic direction as this becomes clearer from a PHM perspective.
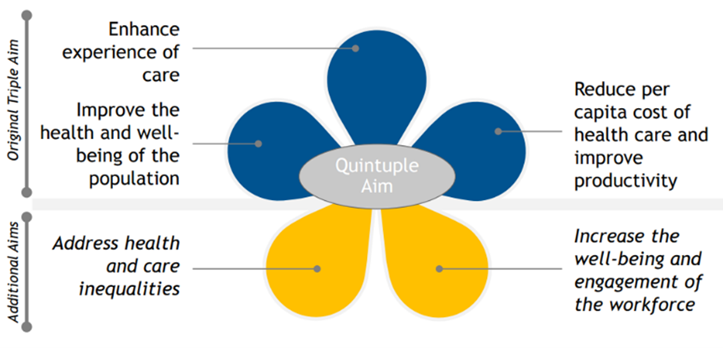
PHM is driven by quintuple aims which build on the triple aim of health care (Figure 1).
Figure 1: Quintuple aims of PHM
A PHM approach starts from the perspective of understanding people, their lives and the impact of health and wellbeing as well as the disease processes on them. PHM enables the system to:
- Use data and intelligence in a systematic way to understand health and care needs, reveal opportunities for improvements in care and set strategic priorities
- Use insights on the population alongside evidence of best practice to develop models of care that improve the health and wellbeing of identified populations and segments
- Adopt integrated models of care and deliver more joined up care for the right people, in the right place at the right time
- Align system wide working and partnership approach
- Deliver targeted and proactive care and support to people through the use of segmentation, stratification and impactability modelling and
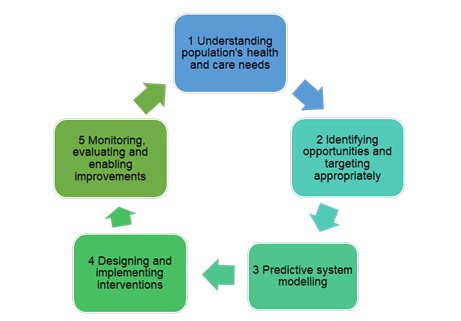
- Support evidence-based decision-making, prioritising collective resources to maximise impact and improve outcomes (Figure 2).
Figure 2: PHM cycle
1.1 Strategic context
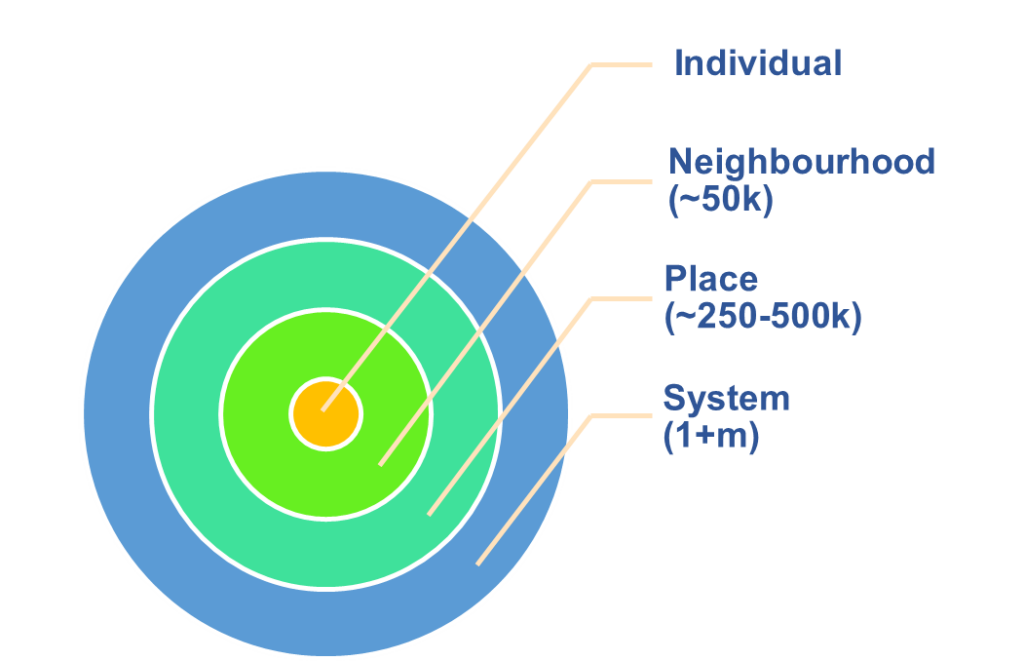
The NHS Long Term Plan (LTP) and the Hertfordshire and West Essex (HWE) Integrated Care System (ICS) Strategy and other strategic documents (e.g. Data Saves Lives) require the ICS to develop and increase the use of PHM as a tool to support the transformation of care and service provision for its population from a developed infrastructure (Figure 3).
Figure 3: Hertfordshire and West Essex (HwE) geography

Health and care organisations work together to build an integrated system that will ensure that we can all live, work and play in healthy and safe communities where everyone’s contributions are valued, and we all have the opportunities and support we need to thrive. This strategy frames the ambition of the HWE ICS to become a system with an advanced PHM capability within the next 2-3 years. It supports the system to extend and embed a responsive PHM approach across its geography and between system, Healthcare Partnership (HCP), neighbourhood and the individual level (Figure 4).
Figure 4: PHM supports different parts of the system
This strategy builds on previous developments across the three former Clinical Commissioning Group areas as well as within the ICS since its formation in July 2022.
2. Embedding PHM Approach within HWE
The foundation for delivering PHM is high quality data, linked at the person level, joining information from different parts of the health and care system. Building on the foundation of a high quality data set, wider PHM infrastructure is required to analyse and interpret the data and generate insights that can be acted on. Our PHM team in the ICB brings together staff with a set of skills and expertise to deliver the PHM function for HwE and support embedding the approach across the system, bridging data and knowledge and enabling solutions that are going to address identified priorities through the use of tools, resources and evidence review.
PHM requires four building blocks, collectively known as the four I’s, i.e. infrastructure, intelligence, intervention and incentive. HWE ICS aims to be an insights-driven ICS with advanced PHM capabilities. This requires an iterative process that improves our capacity and capability through development of infrastructure, intelligence interventions and incentives. The following sections describe the aims for each of the 4 I’s, considering the current position of the ICS and what steps need to be taken. The aims described in the strategy draw on the criteria for a ‘mature’ system as outlined in the PHM Maturity Matrix (NHSE HWE Maturity Matrix Interim Summary Report, February 2024).
2.1 Infrastructure
Aim
- The ICS uses comprehensive information on the population, with data from across the system and tools that support the delivery of all PHM functions
- An intelligence team with skills, capability and capacity to produce insights and support their use across the system
- Supporting self-serve function and enabling people to apply PHM methodology and tools confidently for better decision making
- Ensuring that robust governance and leadership processes are in place to support the delivery of the PHM function
The PHM Strategy sets out the rationale for improving the infrastructure for PHM within the system and the actions necessary to deliver a fully functioning PHM capability. This is both the physical infrastructure as well as the governance, processes and relationships that are needed to effectively deliver PHM. Improving the level of maturity in PHM infrastructure across the ICS will ensure that analysis is accurate and actionable and that the care and support delivered is delivering against the quintuple aims of the health system. In turn this will make best use of the limited resource to deliver PHM within the system and coordinate the work, avoiding duplication of effort.
The table below describes how the ICS will deliver the aims for infrastructure above.
| How will we achieve our aims | Why is it important | Current position in HWE |
| The ICS uses comprehensive information on the population, using data from across the system with tools that support the delivery of all PHM functions | ||
| The ICS will develop a fully functioning PHM platform linking data from across health and care settings, linked at the person level | Longitudinal record provides an integrated view over time rather than a transactional organisational view. | No current single data record. National available tools (e.g. Model Health System, Fingertips etc.). |
| Incorporate non-health data into the linked data set | To understand wider determinants and incorporate wider information into advanced analytics | Social care data not currently flowing, but arrangements are in place for future flows. |
| The data platform incorporates core PHM analytical tools (e.g. segmentation and risk stratification) | To identify target cohorts for care | PHM continues to work with INTs and programmes with current information available until the data platform can be implemented to enhance opportunities. |
| Adopt standardised code sets | Improvement in data quality enhances the ability to analyse data and identify people with risk factors | Tools – Ardens Clinical. Agreed code sets – frailty code sets. |
| Make better use of emerging technologies such as machine learning and artificial intelligence (AI) | To produce bespoke and advanced analytics and support self-serve function | Ongoing work with the University of Hertfordshire will support development of bespoke and advanced analytical capabilities and will give the teams opportunity to access information as they require. |
| An intelligence team with skills, capability and capacity to produce and use insights across the system | ||
| Create a single Intelligence Function for the ICS | Recognise the need for advanced analytics | Huddles, Network and Steering Group meetings are in place with appropriate governance arrangements which support collaborative working. |
| Application of PHM outputs | To enhance the capability for PHM across HWE through the delivery of learning and development | Our PHM Offer supports application of PHM outputs and ensures that teams are enabled to make best use of the available resources. |
| Train and upskill analytical staff using recognised framework (e.g. National Competency Framework) | To support production of outputs with advanced set of analytical tools and skilled analysts | Partnership working with University of Hertfordshire continues to develop our analytical workforce. |
| Drop-in sessions with PHM and Business Intelligence (BI) teams | To support colleagues with data queries and embedding PHM approach in programmes of work | Drop-in sessions are available for colleagues with data queries. These sessions also enable focus on specific work areas. |
| Supporting self-serve function and enabling people to apply PHM methodology and tools confidently for better decision making | ||
| Develop structured reports and dashboards | To allow easy access to information so that teams are enabled and encouraged to embed PHM tools and outputs and can make use of these as part of business as usual for driving improved outcomes | This will emerge and mature with the implementation of the data platform. |
| Training and development of wider workforce | To help teams build confidence in using PHM tools and methodology to move to a population health approach, taking data/analysis specific elements into account | Drop-in sessions are available for colleagues with data queries. These sessions also enable focus on specific work areas. Implementation of the data platform will allow people to access the information they require. |
| Ensuring that robust governance, leadership and processes are in place to support the delivery of the PHM function | ||
| Ability to reidentify individuals | To deliver preventative and personalised care | This will be delivered through the data platform. As an interim measure, HWE are using GP searches to build the bridge from aggregate insights to individual action. |
| Develop existing governance to create broader engagement | To support integrated working across the footprint | Data Platform Board in place with assigned SRO. The ICB Population Outcomes Improvement Committee (POIC) maintains oversight of PHM activity and progress is fedback to the Executive team and the Board that provide strategic steer. The PHM Steering Group and the PHM Network meet regularly to discuss progress regarding ongoing work within the PHM space, inform partners of emerging priorities/programmes of work/requests/plans and agree next steps collectively. The membership of these is partner-wide. The PHM Team works across different footprints (e.g. place / neighbourhood). |
| Linked data sets will be managed in line with Common Law Duty of Confidentiality | Ensuring compliance as per the law | Robust governance processes are being developed with clear accountability. |
| Key activities | Outputs |
| 2024/25 | |
| Making the best use of the data and tools available currently. Implementation of the HWE PHM data platform based on linked data. Embed Outcomes Framework within the above platform. Inclusion of codes sets into contracts and in discussions with providers. Sharing HWE PHM data platform access with providers where IG allows. Training and development of the analytical staff, supported by partnership working with the University of Hertfordshire and the wider resources. | Ongoing publication of insights packs using locally and nationally available data and PHM tools. Single integrated health and care record that features PHM insights, based on the linked data set. |
| 2025/26 | |
| Clear vision for PHM at system and place with fully fledged PHM platform which is understood by decision makers. Creation of a data strategy including social determinants data for expansion of data sets within the HWE PHM data platform. Implementation of self-serve through the use of the data platform outputs of which are understood by decision makers this will be supported by training of wider staff to allow self-serve and application of information. | Clear multi-professional leadership throughout the different tiers of ICS. Ongoing publication of insights packs. |
| 2026/29 | |
| Clear plans for converging shared care records with linked data for PHM. Enabling best use of machine learning and AI. | Developed analytical workforce. Full flows of data from all health and social care sources. Ongoing publication of insights packs. |
2.2 Intelligence
Aim
- Insights support the identification of priorities and opportunities at all levels of the system and are routinely available to end users
- Strategic health system planning uses PHM intelligence to understand current and future need and determine the potential impact of different decisions
- Service development and improvement routinely uses PHM intelligence to design models of care and pathways to target individuals with the greatest need and capacity to benefit
- Different layers of the system use PHM tools to identify target cohorts and individuals that are most likely to benefit from care and support.
Using data and insights supports and informs decision-making and service design by understanding needs of the population and identifying opportunities to improve population outcomes. A system that has a mature PHM Intelligence function will systematically use intelligence and insights to set priorities based on need and future demand, develop evidence-based interventions that target people with the greatest need and potential to benefit. Delivering a mature cross-organisation intelligence function will support the ICS to prioritise effectively and deliver the greatest impact for the resource available.
The table below describes how the ICS will deliver the aims for intelligence above.
| How will we achieve our aims | Why is it important | Current position in HWE |
| Insights support the identification of priorities and opportunities at all levels of the system and are routinely available to end users | ||
| Routinely publish insights packs and produce interactive reports accessible through the data platform | To understand our needs, identify opportunities and agree priorities for action | Overview of the health needs of HWE published for two consecutive years. PCN, locality and place insights packs published. Topic specific insights packs published on a range of conditions. These are published on our PHM website . We have agreed system priorities for HWE using insights from our population. |
| Outcomes Framework | By focussing on our priorities we will improve our population’s health | Approach agreed at Board and POIC 2023-2024. |
| Access to PHM Champions | To help understand findings of the insights packs | The PHM Champions are aligned to specific programmes of work across the system and ensure that data intelligence forms part of programmes of work across the HWE footprint to support improved outcomes for the population. |
| Strategic health system planning uses PHM intelligence to understand current and future need and determine the potential impact of different decisions | ||
| Dynamic system modelling | To support senior leaders to assess current and future demand and impact for HWE population and inform decision making | Partnership working with University of Hertfordshire to model through different scenarios on system-wide demand and capacity modelling. |
| Training and support to staff in understanding, interpreting, and making decisions based on insights | To ensure that staff are able to apply insights available | PHM Champions are aligned to programmes of work. Staff within Medical Directorate are heavily involved in these programmes to support teams in understanding and interpreting these with support on evidence-based decisions. |
| Service development and improvement routinely uses PHM intelligence to design models of care and pathways to target individuals with the greatest need and capacity to benefit | ||
| Using insights to inform programmes of work | To inform ICB and ICS programmes of work through: – deep dive/insights packs for priority areas – modelling of impact to support business case development (e.g. scenario modelling, benefits modelling) – use of PHM tools (e.g. segmentation and risk stratification) to identify target cohorts for care | At programme level, these are used to inform and set programme plans. We used the overview of the population to identify cardiovascular premature mortality as a system priority. Then the insights packs identified key opportunities to improve cardiovascular outcomes which results in hypertension and lipid management workstreams. |
| Using insights to address health and inequalities | To focus on health and inequalities to make improvements for our population by understanding needs of our population from multiple lenses including health inequalities | Ongoing work to address these across the HWE footprint. Implementation of the data platform will allow viewing of information via demography, geography and epidemiology. |
| Impact analysis and scenario modelling are used to assess the benefits and impact of different options | Impact analysis supports decision making by identifying the value of different options and the impact on population health outcomes | Not routinely used across all programmes. Scenario modelling has been used to support the development of business cases across Prevention and Long Term Conditions. |
| Evidence reviews | To ensure that evidence is taken into account when designing care models and pathways | Staff within Medical Directorate are heavily involved in programmes of work and help with evidence review to help support local requirements and interventions. |
| Different layers of the system use PHM tools to identify target cohorts and individuals most likely to benefit from care and support | ||
| Segmentation and risk stratification is used to identify target cohorts for services | To identify target cohorts for care | PHM continues to work with HCPs, INTs and programmes with current information available until the data platform can be implementation to enhance opportunities. |
| Key activities | Outputs |
| 2024/25 | |
| Partnership working with University of Hertfordshire to develop and embed advanced analytical capabilities. Development of shared understanding of priorities identified through the use of insights and intelligence at different tiers of the ICS. Insights to be delivered to strategic, operational and clinical decision makers. Development of workforce to provide system wide capabilities to apply insights. | Shared understanding of priorities. System wide understanding of achievable health and well-being outcomes including mitigated scenarios. |
| 2025/26 | |
| Population health data to be used for forecasting demand based on different scenarios. Analysis shows future demand of segments and identifies those patients who are at greatest risk of a deterioration in health and care. | Move from descriptive to predictive analytics through a combination of tools such as R and Python and skills development. |
| 2026/29 | |
| Costings data. Workforce development and realigning. | Workforce with advanced analytical skills |
2.3 Intervention
Aim
- Service development and improvement routinely uses PHM intelligence to inform and design integrated models of care and pathways with focus on proactive, preventative and early interventions to target individuals with the greatest need and capacity to benefit
- PHM tools help teams work collaboratively and there are clear working arrangements to improve our population outcomes through programmes and to be delivered via HCPs and INTs to develop models of care and pathways that triangulate insights from analysis, with evidence of best practice and local perspectives from clinicians, patients and the public
- Progress in reducing health inequalities
- Understanding impact of services, models of care and interventions on required outcomes, demonstrating value and building on best practice evidence
Design of care models that are shaped around the needs of the population and the identified opportunities ensure delivery of proactive and responsive integrated care models. Use of best practice evidence supports the ICS/ICB programmes of work and ensure that resources are focussed on high impact interventions that are tailored around the right cohort of individuals. This will help ensure that we are able to demonstrate value and make progress on reducing inequalities.
The table below describes how the ICS will deliver the aims for intervention above.
| How will we achieve our aims | Why is it important | Current position in HWE |
| Service development and improvement routinely uses PHM intelligence to inform and design models of care and pathways with focus on proactive, preventative and early interventions to target individuals with the greatest need and capacity to benefit | ||
| Support for senior leadership and executive teams for informed decisions | To support senior decision-making on implementation of appropriate models of care, pathways and interventions to improve population health | Our PHM insights have informed the ICB Clinical Priorities that have been signed off. These are used to inform programmes of work. |
| Using insights to inform programmes of work | To inform ICB and ICS programmes of work at different levels in the system through: – deep dive/insights packs for priority areas – modelling of impact to support business case development (e.g. scenario modelling, benefits modelling) – use of PHM tools (e.g. segmentation and risk stratification) to identify target cohorts for care | At programme level, these are used to inform and set programme plans. We used the overview of the population to identify cardiovascular premature mortality as a system priority. Then the insights packs identified key opportunities to improve cardiovascular outcomes which results in hypertension and lipid management workstreams. PHM team supports working with ICS and place teams to understand and respond to needs through close working with other teams e.g Medical Directorate to identify best practice interventions. |
| Using insights to address health and inequalities | To focus on health and inequalities to make improvements for our population | Ongoing work to address these across the HWE footprint. |
| Impact analysis and scenario modelling are used to assess the benefits and impact of different options | Impact analysis supports decision making by identifying the value of different options and the impact on population health outcomes. | Not routinely used across all programmes. Scenario modelling has been used to support the development of business cases across Prevention and Long Term Conditions. |
| PHM tools help teams work collaboratively and there are clear working arrangements to improve our population outcomes through programmes and to be delivered via HCPs and INTs to develop models of care and pathways that triangulate insights from analysis, with evidence of best practice and local perspectives from clinicians, patients and the public | ||
| Widespread use of logic models and evidence-based design | To support planning and development of targeted services by creating a link between identified opportunities/challenges, defining the issue that is being addressed, identifying the outcomes of interest and reviewing the evidence of what works to deliver maximum value To create a strong case for change | Not yet widely adopted or systematic but logic models are being used to support the development of interventions in INTs and across ICS programmes. The approach was used to help identify who are most likely to benefit and the evidence to design new models of care and clinical pathways for the management of people with poor lipid control. This informed the outcomes we are seeking to improve for this cohort. |
| Insights are used to identify how multi-agency working can deliver improved health outcomes for the population | To support integrated care design for improved population outcomes | INT working has been successful in embracing and ensuring multi-agency working. Work continues to evaluate the impact. |
| Progress in reducing health inequalities | ||
| Providers and service teams can use PHM tools, including the ability to reidentify individuals to target people experiencing health inequalities | To reidentify specific individuals in at risk / segmented cohorts for directed interventions | Implementation of the data platform will allow data to be viewed through different lenses. ICS programmes of work focuses on specific components of Core20+5 requirements. |
| Understanding impact of services, models of care and interventions on required outcomes, demonstrating value and building on best practise evidence | ||
| Monitoring and evaluation | To understand impact, demonstrate value, feed into continuous improvement cycle | Engagement with programme leads continues to identify evaluation resources/tools currently being used by teams as well as barriers and facilitators to incorporating evaluation into projects. This will inform the development of the Evaluation Framework. The PHM Strategy operates in close collaboration with the HWE Research and Innovation Strategy. Both of these recognise the value and importance of embedding evaluation early on within teams, processes and programmes of work for driving sustainable improvements. System wide adoption of the ICS Outcomes Framework will help measure impact of our interventions. |
| Assessment of inequalities | To assess inequalities and variation with a view to improve | Implementation of the data platform continues to enable this – viewing data through different lenses. |
| Supporting ICS and its partners with their functions, priorities and informed decision making | Using what works, where improvements are required to maximise value, improve access and experience and focus on where services can deliver improved outcomes/impact To enable workforce, finance, quality and performance planning To inform commissioning processes | Fragmented approach to evaluation currently. Development of Evaluation Framework continues. |
| Key activities | Outputs |
| 2024/25 | |
| Partnership working with University of Hertfordshire and Medical Directorate to embed best practice evaluation across our programmes. Development of shared understanding of priorities identified through the use of insights and intelligence at different tiers of the ICS e.g. HCP and PCN / INTs. Embed the use of the Outcomes Framework to understand impact of interventions. Engagement with programmes to understand tools current processes around evaluation and barriers if not present. Development of Evaluation Framework along with the Research and Innovation Strategy. | Programmes are based on best practice interventions identified as needs through insights packs with developed logic models that are supported by evaluation impact reported through programme governance Use of evidence and impact in decision making. |
| 2025/26 | |
| Development of logic models across the ICS to build the foundations for evaluation. Defined care models in place for the different programmes / population groups. Implementation of the Evaluation Framework. | Robust processes and infrastructure in place supporting evaluation. Use of evidence and impact in decision making. |
| 2026/29 | |
| Continuing to refine outputs from the scenario modelling work developed in partnership with the University of Hertfordshire | Use of evidence and impact in decision making |
2.4 Incentives
Aim
- The ICS uses PHM to ensure that resources are allocated efficiently and deliver the greatest value and outcomes
- Payment models are structured around current and future health needs and populations, rather than organisations and services
- Workforce development and realignment
Creating shared accountability for improving outcomes based on needs of our population supports incentives that are population-centred and ensures a joined-up approach across the whole of the footprint.
Accountability Framework
The system uses an Accountability Framework to align funding and financial incentivisation to outcomes with the population. Adopting the PHM approach will enable the ICS to develop a population focussed Accountability Framework. This will be based on ensuring evaluation of delivery of outcomes. HCPs, in particular, will be supported with focussing their activities on key areas that will bring the biggest value through the PHM approach. We have been going through the process of developing population health indicators across programme by programme which will help deliver population health outcomes for HWE. Work is ongoing to populate these with baselines and gauge the level of ambition for each of our HCPs.
The table below describes how the ICS will deliver the aims for incentives above.
| How will we achieve our aims | Why is it important | Current position in HWE |
| The ICS uses PHM to ensure that resources are allocated efficiently and deliver the greatest value and outcomes | ||
| Development of HWE Segmentation model including Patient Level Information and Costing System (PLICS) data to be delivered as part of the HWE PHM data platform implementation | To help maximise use of resources and improve efficiencies | Data platform implementation continues. |
| Payment models are structured around current and future health needs and populations, rather than organisations and services | ||
| Creating an Accountability Framework that is structured around the population and ICS programmes of work | To align funding and financial incentivisation to outcomes with the population | This is under development and the Outcomes Framework will form the basis of this. |
| Incorporate population health metrics into the Accountability Framework | To ensure that local services and service development not only deliver high performance and high quality, but also deliver improvements in health outcomes | The approach has been signed off by Board and POIC. We are working with teams to develop baseline and ambitions for our programme outcomes and embedding this as part of HCP Accountability Framework. |
| The system is aligned to the delivery of outcomes in the Accountability Framework, with targets and ambitions set with funding and investment aligned to delivery | To incentivise delivery of improved outcomes, not just delivery of more activity | PHM team with BI and Oracle will include dashboards as part of implementation. |
| Investment and incentives consider opportunities that offer the greatest return on investment, taking both current and future demand into account | To ensure greatest value and focus on areas with the greatest benefit | Currently developing and data platform implementation will support. |
| Workforce development and realignment | ||
| Upskilling teams and realigning | To ensure our workforce is supported to deliver outcomes for our population through enhanced capabilities | We are working on the development of our intelligence function to support our vision and activities. Our workforce is given the opportunity to develop partnership working with the University of Hertfordshire. This has been useful in developing relationships and gaining new experience. This is a step forward for upskilling teams and ensuring that teams are aligned appropriately. |
| Key activities | Outputs |
| 2024/25 | |
| Delivery of the segmentation model as part of the HWE PHM data platform. Embed PLICS data as part of the expansion of data sources for HWE PHM data platform. | Usage of data platform |
| 2025/26 | |
| Develop method and assumptions to build finance and baseline model that maps to the Outcomes Framework. | The ability for programmes to measure improvements in outcomes |
| 2026/29 | |
| Develop priority areas to understand and review allocation of resources. Testing new funding models to reallocate resources to greatest need. | Resources are allocated and utilised efficiently and effectively |
3. Concluding remarks
Adopting the PHM methodology can provide information on current and future health and care needs and help bridge the gap between evidence and action on how to address them. Through PHM, we can identify what the greatest opportunities are for improving the health and wellbeing of our population, both mentally and physically to design and implement proactive and preventative services and interventions for the right cohort of individuals where they are needed the most across organisations. We recognise that improvements cannot be delivered by one part of our system alone. Our PHM approach supports collaboration between health and care services across HWE. This approach provides assurance on how efficiently national, local and organisational requirements are being delivered in HWE through the use of data, insights, intelligence and evidence-based best practice. Evaluation is a key part of this process, allowing teams to monitor progress, learn and adapt as necessary so that we can ensure responsiveness of our health and care system to the changing needs of the population and demonstrate value.
Primary care network packs
There are PCN-level packs available for this year and previous years across our three places:
Overview of the population
You can find files relating to our health needs analysis on this dedicated page.
Programmes
Cancer
Children and young people
Frailty and end of life
Long-term conditions (diabetes and cardiovascular disease)
Mental health / learning disabilities
Planned care
Prevention
Unplanned care
Sub-geography
Evaluation
Evaluation offers a way to determine whether an initiative has been worthwhile in terms of delivering what was intended and expected. It is particularly helpful to inform future developments. Therefore, a quick guide has been put together for staff to help them plan for evaluation at the beginning of any project and the support that is available to them. Please use the quick guide below.
Evaluation v0.01 dated March 2025_UPDATED_website (191kB pdf)
Wider Tools and Resources
Hertfordshire County Council JSNA / evidence and insights Essex County Council JSNA / evidence and insights Fingertips Model health system (this requires approved access) Cardiovascular disease Prevent PaPI (this requires approved access) FDP/Foundry (this requires approved access)PHM newsletters and case studies
You can read our newsletter and find case studies here.
Our communities
he Hertfordshire and West Essex ICS (Integrated Care System) area is made up of a mix of large and small towns, villages and countryside, with a growing and increasingly diverse population.
Essex data
You can find detailed information about Essex’s communities, from population statistics to data on highways use and social care on the Essex Open Data pages of the Essex County Council website.
Hertfordshire data
You can find detailed statistical information about Hertfordshire’s communities and the people who live in them on the Herts Insight pages of the Hertfordshire County Council website.
Census 2021
The first release of information from the Census 2021 has now been published.
Find out more about what information will be released and when, on the Office for National Statistics Census 2021 website.